Endometriosis
Highlights
Endometriosis Symptoms
Endometriosis symptoms vary widely, and some women with the condition have no symptoms. Symptoms can include:
- Pelvic pain, especially around the time of menstruation
- Pain during sexual intercourse
- Heavy menstrual bleeding
- Sleep problems
- Cyclical abdominal pain
- Intermittent diarrhea and constipation
- Painful or difficult urination
- Blood in the urine
Infertility and Endometriosis
Endometriosis rarely causes a complete inability to conceive, but it can contribute to reduced fertility both directly and indirectly.
Treatment
Treatment options for endometriosis include:
- Watchful Waiting. Delaying treatment may be most appropriate for women with mild endometriosis or those who are approaching the age of menopause.
- Drugs. First-line drug therapies are estrogen-progestin oral contraceptives, which are usually used along with nonsteroidal anti-inflammatory drugs (NSAIDs). Progestin-only pills, injections, or intrauterine device (IUD) may also be used. Gonadotropin-releasing hormone (GnRH) agonist drugs are another option.
- Surgery. Conservative surgery approaches, such as laparoscopic ablation, remove endometrial implants and cysts but do not remove reproductive organs. Conservative surgery can help improve fertility. Hysterectomy, the surgical removal of the uterus, may be recommended in severe cases of endometriosis, but it does not necessarily cure the condition.
Introduction
Endometriosis is a condition in which the cells that line the uterus grow outside of the uterus in other areas, such as the ovaries. The condition can interfere with a woman's fertility and ability to become pregnant. Endometriosis can also cause severe pelvic pain, especially during menstruation.
Endometriosis is a common gynecological condition. It is chronic, and may be a painful and progressive disease. However, the causes of endometriosis are unknown, it is widely variable in symptoms and severity, and it is difficult to diagnose.
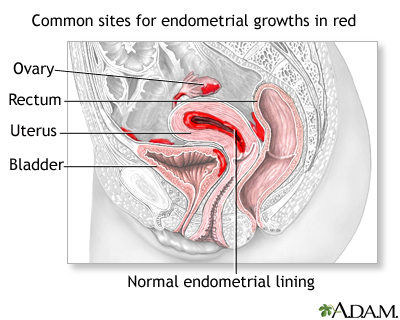
Endometrial Implants
Endometriosis occurs when cells from the tissue layer lining the uterus (endometrium) form implants that attach, grow, and function outside the uterus, generally in the pelvic region.
Endometrial cells contain receptors that bind to estrogen and progesterone, which promote uterine growth and thickening. When these cells become implanted in organs and structures outside the uterus, these hormonal activities continue to occur, causing bleeding and scarring.
Endometrial implants vary widely in size, shape, and color. Over the years, they may diminish in size or disappear, or they may grow.
- Early implants are usually very small and look like clear pimples.
- If they continue to grow they may form flat injured areas (lesions), small nodules, or cysts called endometriomas, which can range from sizes smaller than a pea to larger than a grapefruit.
- Implants also vary in color; they may be colorless, red, or very dark brown. These so-called chocolate cysts are endometriomas filled with thick, old, dark brown blood. They usually appear on the ovaries.
Location of Implants
Implants can form in many areas, most commonly in the following locations in the pelvis:
- Ovaries
- Fallopian tubes
- Uterine surface
- Cul-de-sac, an area between the uterus and rectum
- Bowel
- Bladder
- Rectum
- The peritoneum. This is the smooth surface lining that covers the entire wall of the abdomen and folds over inner organs in the pelvic area.
Rarely, remote sites of endometriosis may include the spinal column, nose, lungs, pelvic lymph nodes, the forearm, and the thigh.
Process of Endometriosis
The process of endometriosis mimics menstruation at certain stages:
- Each month, the exiled endometrial implants respond to the monthly cycle just as they would in the uterus. They fill with blood, thicken, break down, and bleed.
- Products of the endometrial process cannot be shed through the vagina as are menstrual blood and debris. Instead, the implants develop into collections of blood that form cysts, spots, or patches.
- Lesions may grow or reseed as the cycle continues.
The lesions are not cancerous, but they can develop to the point that they cause obstruction or adhesions (web-like scar tissue) that attach to and bind together nearby pelvic organs, causing pain, inflammation, and sometimes infertility.
Causes
Doctors don’t know the exact cause of endometriosis. A combination of genetic, biologic, and environmental factors may work together to trigger the initial process, produce implantation, and cause subsequent reseeding and spreading of the implants.
Theories of the cause of endometriosis include:
- Retrograde Menstruation. Retrograde menstruation occurs during a woman's period, when menstrual tissue flows backward through the fallopian tubes rather than out through the vagina. In some cases, the redistributed endometrial tissue may attach and grow in areas outside the uterus, forming endometriosis implants. This theory does not fully explain endometriosis, however. Many women have some retrograde menstruation, but not all of them develop endometrial cysts. Consequently, other factors must explain why uterine tissue becomes implanted and grows in areas outside the uterus.
- Exposure to Estrogen. Prolonged exposure to estrogen may play a role in the development of endometriosis. Causes of prolonged exposure to the body’s own estrogen include early-age menstruation, short menstrual cycles, and obesity. Sources of external estrogen exposure include endocrine-disrupting chemicals.
- Impaired Immune System. Another theory is that women who develop endometriosis have an impaired immune system that fails to identify and destroy endometrial tissue that grows outside of the uterus. Some researchers think that endometriosis is a type of autoimmune condition, in which the immune system launches an attack on its own cells and tissue. There appears to be a relatively high incidence of other inflammatory autoimmune disorders (such as multiple sclerosis, rheumatoid arthritis, and lupus) among women with endometriosis. It is unclear, however, how this response relates to endometriosis itself and whether endometriosis should be treated as an autoimmune condition.
- Inflammatory Response. The damage, infertility, and pain produced by endometriosis may be due to an overactive response by the immune system to the early presence of endometrial implants. The body, perceiving the implants as hostile, launches an attack. Levels of large white blood cells called macrophages are elevated in endometriosis. Macrophages produce very potent factors, which include cytokines (particularly those known as interleukins) and prostaglandins. Such factors are known to produce inflammation and damage in tissues and cells.
Risk Factors
About 5 million American women have endometriosis.
Age
Endometriosis can occur in teenagers and adult women of all ages, but most typically it occurs in women ages 25 - 40.
Family History
A family history of endometriosis, especially in a mother or sister, increases a woman’s likelihood of developing it herself.
Not Having Had Children
Pregnancy appears to be protective against endometriosis, while never having had children is associated with increased risk. However, endometriosis can still occur in women who have had children.
Dietary Factors
Some studies suggest that consumption of red meat and trans fats may increase the risk of developing endometriosis, while consumption of fruits, green leafy vegetables, and omega-3 fatty acids (found in fish) may be protective.
Menstrual History
Women at increased risk for endometriosis tend to have more problems with menstruation. They usually have a shorter than normal cycle, heavier periods, and longer periods. They may also have begun menstruating at a younger than average age.
Complications
Pain
Adhesions can cause significant pain. They are dense, web-like structures of scar tissue that can attach to nearby organs. Pelvic pain is the most common complaint for women with endometriosis, and it can significantly impair the quality of life, including work and social activities. The pelvic pain associated with endometriosis is usually chronic (lasting more than 6 months). Pain may also occur in the abdomen and back.
Infertility
Infertility is another main complication of endometriosis. Endometriosis is responsible for about a third of cases of female infertility. Endometriosis rarely causes an absolute inability to conceive, but it can reduce fertility both directly and indirectly:
- If implants occur in the fallopian tubes, they may block the egg's passage.
- Implants that occur in the ovaries prevent the release of the egg.
- Adhesions that form among the uterus, ovaries, and fallopian tubes can prevent the transfer of the egg to the tube.
Effects on Other Parts of the Pelvic Region
Implants can also occur in the bladder (although less commonly) and cause pain and even bleeding during urination. Implants also sometimes form in the intestine and cause painful bowel movements, constipation, or diarrhea.
Symptoms
Not all women with endometriosis have symptoms. When symptoms occur, pain is the main one.
Many women with endometriosis have chronic pain in the pelvic area (the lower part of the trunk of the body). The pain is often a severe cramping that occurs on both sides of the pelvis, radiating to the lower back and rectal area and even down the legs. The pain may be continuous or it may come and go. Pain tends to worsen over time.
The severity of the pain varies widely and does not appear to be related to the extent of the endometriosis itself. In other words, a woman can have very small or few implants and have severe pain, while those with extensive endometriosis may have very few signs of the disorder except for infertility. Large cysts can rupture and cause very severe pain at any time.
Pain caused by endometriosis is associated with:
- Menstruation. Women with endometriosis typically have heavy or prolonged menstrual bleeding, and very painful menstrual cramps (dysmenorrheal). Women may also experience pelvic pain at other times during their menstrual cycle and they may have spotting or bleeding between periods. Menstrual pain may worsen over time.
- Sexual Intercourse. Endometriosis can cause pain during or after sexual intercourse (dyspareunia).
- Urination and Bowel Movements. Pain during defecation or urination may be especially severe during menstrual periods. Women may also experience other gastrointestinal problems, such as diarrhea, constipation, or bloating.
Diagnosis
Because endometriosis symptoms do not always appear, or may be caused by other conditions, a diagnosis cannot be based on symptoms alone. Laparoscopy, an invasive diagnostic procedure, is the only definitive method for diagnosing endometriosis. However, a trial using a hormonal drug may be used to confirm or rule out endometriosis.
Pelvic Exam
After collecting your symptom report and medical history, the doctor will perform a physical and pelvic exam. During the pelvic exam, the doctor will evaluate the size and position of the ovaries and check for tender masses or nodules behind the cervix.
Laparoscopy
Diagnostic laparoscopy is used to confirm a suspected diagnosis of endometriosis and to evaluate the severity of the condition. It may also be used to treat endometriosis. During laparoscopy, the surgeon determines the number, size, and location of endometrial implants and adhesions. This information can help in staging endometriosis and in making treatment decisions.
The procedure involves the doctor making a small incision in the abdomen, and inserting a thin flexible fiber-optic tube (the laparoscope). The laparoscope is equipped with a small telescopic lens, which enables the doctor view the uterus, ovaries, tubes, and peritoneum (lining of the pelvis) on a video monitor. Laparoscopy normally requires a general anesthetic, although the patient can go home the same day. [For more information on laparoscopy, see the "Conservative Surgery" section of this report.]
Imaging Tests
An ultrasound is performed in cases where other conditions are suspected, such as uterine fibroids, ovarian cysts, or ectopic pregnancy. This non-invasive imaging technique can detect endometriomas, cysts that are usually located on the ovaries and filled with thick dark blood. Ultrasound can also pick up cysts larger than 1 cm (about 1/3 inch), but it will miss smaller cysts, or small and shallow endometrial implants on the surface of ovaries or on the peritoneum (lining of the pelvis). Other imaging techniques, such as computed tomography (CT) scanning or magnetic resonance imaging (MRI), may occasionally be used.
Ruling out Conditions with Similar Symptoms
Many conditions cause pelvic pain. In many cases, the cause is unknown, and the condition often resolves on its own. However, some causes of pelvic pain can be serious and should be ruled out during a work-up for endometriosis.
Primary Dysmenorrhea. Primary dysmenorrhea is recurrent pelvic pain associated with menstruation. Dysmenorrhea is common in many women.
Adenomyosis. A condition called adenomyosis occurs when nodules (knots) of endometrial tissue develop within the deep muscle layers of the uterus. This disorder is often classified with endometriosis, but adenomyosis is a different disease. (Endometriosis occurs when endometrial tissue grows and functions outside the uterus.) Adenomyosis is a significant cause of severe pelvic pain and menstrual irregularities. It typically occurs in women who have uterine fibroids, women age 40 - 50, and women who have had children. Women who have had surgery for endometriosis, yet continue to suffer from menstrual and pelvic pain, may actually have adenomyosis.
Other Causes of Pelvic Pain. Many conditions cause pelvic pain that may or may not be related to menstruation. Some causes of pelvic pain that can be serious and should be ruled out include:
- Uterine fibroids
- Pelvic inflammatory disease (which is a result of infections in the pelvic area)
- Miscarriage
- Ectopic pregnancy (when the fertilized egg implants in an area outside of the uterus, usually the fallopian tube)
- Pelvic cancer (rare)
- Uterine polyps
- The use of an intrauterine device (IUD) for contraception
Conditions that may mimic symptoms of endometriosis but which are unrelated to problems in the reproductive organs include:
- Severe kidney or urinary tract infections
- Celiac disease
- Appendicitis
- Interstitial cystitis
- Inflammatory bowel disease
- Diverticulitis
- Irritable bowel syndrome
Treatment
There is no perfect way of managing endometriosis. The three basic treatment approaches are:
- Watchful waiting (conservative therapy to relieve symptoms)
- Hormonal therapy (to reduce the size of endometrial implants)
- Surgery (to reduce endometrial implants, restore fertility, or possibly cure the condition)
The choice depends on a number of factors, including the woman's symptoms, her age, whether fertility is a factor, and the severity of the disease.
Watchful Waiting
Delaying treatment may be most appropriate for women with mild endometriosis or those who are approaching the age of menopause.
Women may also use lifestyle modifications, such as exercise and relaxation, to cope with their pain. Nonsteroidal anti-inflammatory drugs (NSAIDs) -- such as ibuprofen (Advil, Motrin, generic) and naproxen (Aleve, generic), or acetaminophen (Tylenol, generic) -- can help provide some pain relief.
Hormonal Therapy
Hormonal therapies are used to mimic states in which ovulation does not occur (such as pregnancy or menopause) or to directly block ovulation. Hormonal drugs include oral contraceptives (a first-line treatment), progestins, GnRH agonists, and (rarely) danazol. They can be very effective in relieving endometriosis symptoms, especially pain. Some of these drugs may also be used after surgery to help prevent recurrence of endometriosis. Downsides of these drugs include:
- None of these drugs can cure the problem. Symptoms recur in about half of patients within 5 years of treatment.
- They do not improve fertility rates and may delay conception.
- Side effects of some of these drugs can be distressing.
- Women who take GnRH agonists, danazol, or similar drugs should use non-hormonal barrier birth control methods (such as the diaphragm, cervical cap, or condoms) because these drugs can increase the risk for birth defects.
Surgery
Surgery is an option for women who:
- Have severe pain that does not respond to watchful waiting and medical treatment.
- Want to become pregnant and endometriosis is most likely the major contributor to infertility.
There are two basic surgical approaches for endometriosis:
- Conservative Surgery (Laparoscopy or Laparotomy). Conservative surgery uses minimally invasive laparoscopy, or sometimes laparotomy (conventional “open” surgery through normal incision), to remove the endometriosis implants without removing any normal tissue or reproductive organs. It is a good option for women who wish to become pregnant or who cannot tolerate hormone therapy. Endometriosis often recurs after conservative surgery, however. The risk for recurrence or residual pain after any procedure increases with the severity of the condition, particularly if endometriosis has affected areas outside the uterus.
- Radical Surgery (Hysterectomy). Hysterectomy offers the best option for either a cure or more significant control of the problem. Younger patients can often have only a hysterectomy while leaving one or both of their ovaries intact. However, if endometriosis has developed outside the uterus then even this procedure is not curative. Removing only the uterus with hysterectomy has the same risk for recurrence as conservative surgery. Removing both ovaries (bilateral oophorectomy) along with the uterus is the only potential cure for endometriosis.
In choosing between hysterectomy (with or without removal of the ovaries) and conservative surgeries, age and the desire for children are important factors.
Nerve Surgery for Pelvic Pain. Laparoscopic uterine nerve ablation (LUNA) and laparoscopic presacral neurectomy (LPSN) are procedures that aim to reduce chronic pelvic pain by destroying or interrupting the nerves that attach the uterus to the pelvic bone. Some small studies have shown more benefit for LPSN than for LUNA. LPSN appears to work best when combined with laparoscopic ablation of endometrial implants (conservative surgery). Stronger evidence is needed before these procedure scan be recommended for women with chronic pelvic pain associated with endometriosis. Many insurance companies consider these procedures experimental and will not pay for them.
Treating Infertility in Patients with Endometriosis
For women with severe endometriosis who want to become pregnant, conservative surgery (typically laparoscopy) is the appropriate approach for restoring fertility. Hormonal therapies that treat endometriosis itself, such as GnRH agonist or progestins, generally do not help fertility. If surgery fails, fertility drugs and assisted reproductive technologies, such as in vitro fertilization, are options. Women with endometriosis who are trying to conceive should discuss all treatment options with a fertility specialist.
Herbs and Supplements
Some studies suggest that the omega 3 fatty acids found in fish and fish oil supplements may be helpful for endometriosis. Others have indicated possible benefits from Chinese herbal medicine. There are few well-conducted studies on these treatments and more research is needed.
Generally, manufacturers of herbal remedies and dietary supplements do not need approval from the Food and Drug Administration (FDA) to sell their products. Just like with drugs, herbs and supplements can affect the body's chemistry, and therefore have the potential to produce side effects that may be harmful. There have been a number of reported cases of serious and even lethal side effects from herbal products. Patients should check with their doctor before using any herbal remedies or dietary supplements.
Medications
The basic approach in hormonal treatments for endometriosis is to block production of female hormones (estrogen and progesterone) or to prevent ovulation. Hormonal drugs are used for pain relief only. They do not improve fertility rates and in some cases may delay conception. Specific hormonal drugs may have different effects for women with endometriosis.
- Inducing Pseudopregnancy. Oral contraceptives that contain estrogen and a progestin mimic a pregnant state and block ovulation. (Progestins are synthetic forms of progesterone). Progestin may also be used alone, since it has specific effects that can cause the endometrial tissue to atrophy (shrink).
- Inducing Pseudomenopause. Gonadotropin-releasing hormone (GnRH) agonists reduce estrogen and progesterone to their lowest levels.
- Inducing On-going Blockage of Ovulation. Danazol, a derivative of male hormones, is a powerful ovulation blocker but has very unpleasant side effects. It is rarely used now.
Most women achieve pain relief after taking these drugs. To date, comparison studies have found few differences in effectiveness among the major hormonal treatments. Differences occur mostly in their side effects. Women should discuss the effects of particular medications with their doctors to determine the best choice.
Oral Contraceptives
Oral contraceptives (OCs), commonly called birth control pills or "the Pill," contain combinations of an estrogen and a progestin. Combined oral contraceptives are a first-line treatment for endometriosis pain. They are generally used along with nonsteroidal anti-inflammatory drugs (NSAIDs) such as ibuprofen.
When used throughout a menstrual cycle, OCs suppress the actions of other reproductive hormones (luteinizing hormone [LH] and follicle stimulating hormone [FSH]) and prevent ovulation. There are many brands available. The estrogen compound used in most oral contraceptives is estradiol. Many different progestins are used, and there are many brands. None to date have proven to be better than others. Women should discuss the best options for their individual situations with their doctor.
Standard OCs are the first-line treatment. They come in a 28-pill pack that contains 21 active pills and 7 inactive pills. Women with severe pain who have not been helped by standard combination OCs may benefit from switching to newer continuous-dosing combination OCs. Continuous-dosing oral contraceptives aim to reduce -- or even eliminate -- monthly periods and thereby prevent the pain and discomfort that often accompanies menstruation. These OCs contain a combination of estradiol and the progestin levonorgestrel but use extending dosing of active pills.
OCs with continuous dosing include:
- Seasonale, contains 81 days of active pills followed by 7 days of inactive pills. Women have on average a period every 3 months.
- Seasonique produces about 4 periods a year. A woman takes 84 days of levonorgestrol-estradiol pills followed by 7 days of pills that contain only low-dose estradiol.
- Lybrel, supplies a daily low dose of levonorgestrel and estradiol with no inactive pills. Because it contains only active pills, which are taken 365 days a year, it completely eliminates monthly menstrual periods, although some women may continue to have occasional bleeding or spotting during the first few months.
Estrogen and progestin each cause different side effects. The most serious side effects are due to the estrogen in the combined pill. Uncommon but more dangerous complications of OCs include high blood pressure and deep-vein blood clots (thrombosis), which may contribute to heart attack or stroke.
Progestins
Progestin alone may be helpful for women whose pain has not been relieved with combination estrogen-progestin oral contraceptives. Progestins can prevent ovulation and reduce the risk for endometriosis in the following ways:
- They block luteinizing hormone (LH), one of the reproductive hormones important in ovulation.
- They change the lining of the uterus and eventually cause it to atrophy.
- They may provide pain relief equivalent to the more powerful hormone drugs. Some doctors recommend them as the first choice for women with endometriosis who do not want to become pregnant.
Specific Progestins. Progestins are available in various forms. They include:
- Intrauterine Device. The levonorgestrel-releasing intrauterine system, or LNG-IUS (Mirena) is very effective for treating heavy menstrual bleeding (menorrhagia), and studies indicate that it helps control the symptoms of minimal-to-moderate endometriosis pain. Progestin released by the IUD mainly affects the uterus and cervix and causes fewer widespread side effects than other forms of progestins. Studies indicate that the LNG-IUS works as well as GnRH agonists in managing endometriosis pain, and causes less loss of estrogen.
- Injection. Medroxyprogesterone (Depo-Provera, also known as DMPA) is administered by injection every 3 months. (A low-dose formulation is called Depo-subQ Provera 104.) Depo-Provera can cause loss of bone mineral density, a condition associated with osteoporosis, but GnRH agonists may cause even more bone thinning. Depo-Provera can cause persistent infertility for up to 22 months after the last injection.
- Pill. Oral progestins include medroxyprogesterone (Provera) and norethindrone (Micronor, Aygestin, Norlutate). Norethindrone is also known as norethisterone.
Side Effects of Progestins. Side effects of progestin occur in both the combination oral contraceptives and any contraceptive that uses only progestin, although they may be less or more severe depending on the form and dosage of the contraceptive. The most common side effects include:
- Changes in uterine bleeding, such as higher amounts during periods, spotting and bleeding between periods (called break-through bleeding), or absence of periods
- Weight gain
- Water retention and swelling in the face, ankles, or feet
- Breast tenderness
- Headaches
- Nausea
- Mood changes
GnRH Agonists
Gonadotropin releasing hormone (GnRH) agonists are effective hormone treatments for endometriosis. They block the release of the reproductive hormones LH (luteinizing hormone) and FSH (follicular-stimulating hormone). As a result, the ovaries stop ovulating and no longer produce estrogen. Ovulation and menstruation resume around 4 - 10 weeks after stopping the drug. The specific length of time depends on the type of GnRH agonist used.
Specific GnRH Agonists. GnRH agonists include the implant goserelin (Zoladex), a monthly injection of leuprolide (Lupron, Depot, generic), and the nasal spray nafarelin (Synarel).
Side Effects and Complications. Common side effects (which can be severe in some women) include menopause-like symptoms, including hot flashes, night sweats, vaginal dryness, weight change, and depression. The side effects vary in intensity depending on the GnRH agonist. They may be more intense with leuprolide and persist after the drug has been stopped.
The most important concern is possible osteoporosis from estrogen loss. To help protect the bones, doctors prescribe “add-back therapy,” with a supplement of combination estrogen-progestin. Because of estrogen loss side effects, doctors generally recommend that women not take GnRH agonists for more than 6 months.
GnRH treatments can increase the risk for birth defects. Women who are taking GnRH agonists should use non-hormonal birth control methods, such as the diaphragm, cervical cap, or condoms while on the treatments.
Other Drug Treatments
Danazol. Danazol (Danocrine, generic) is a synthetic drug that resembles a male hormone (androgen). It suppresses the pathway leading to ovulation. Many women stop taking this drug because of its adverse side effects, which include bloating, acne, irregular vaginal bleeding, and muscle cramps. Danazol can also cause male characteristics, such as growth of facial hair, reduced breasts, and deepening of the voice. Because GnRh agonists cause far fewer side effects, danazol is rarely used these days for endometriosis treatment.
Conservative Surgery
The goal of conservative surgery is to aggressively remove as many endometrial implants and cysts as possible without causing surgical scarring and subsequent adhesions that could cause fertility problems. Surgery can help improve fertility in women with severe endometriosis. Whether it offers any advantage in pregnancy rates in women with mild-to-moderate endometriosis is unclear. Conservative surgery can also help relieve pain caused by implants. It may, however, miss microscopic implants that could continue to cause pain and other symptoms after the procedure.
The two conservative surgical procedures are:
- Laparascopy is the gold standard and most commonly performed surgical treatment for endometriosis. It involves several small abdominal incisions through which a thin telescopic tube (laparoscope) is inserted. The doctor removes implants and scar tissue and destroys them with heat. Laparoscopy requires general anesthesia, but it is an outpatient procedure and the patient can go home the same day. Recovery usually takes a few weeks.
- Laparotomy uses a wide abdominal incision and conventional surgical instruments. It is much more invasive and requires a longer recovery time (typically several months). Laparotomy is rarely performed except in cases of severe endometriosis.
Laparoscopy Procedure
A laparoscopy is performed, usually under general anesthesia, as follows:
- Carbon dioxide gas is injected into the abdomen, distending it and pushing the bowel away so that the doctor has a wider view.
- The procedure requires making small incisions at the navel and above the pubic bone.
- The laparoscope (a narrow tube equipped with camera lenses and a fiber-optic light source) is inserted through the incision at the navel (the umbilical incision).
- A probe is then inserted through the second incision, allowing the doctor to directly view the outside surface of the uterus, fallopian tubes, and ovaries.
- One or two additional small incisions can be made on either side of the lower abdomen through these incisions. Surgical instruments or other devices are passed through these accessory incisions to destroy or remove abnormal tissue. Implants can be removed by excision (surgical removal) using a laser or scissors or by destroying the area with lasers or with electricity (or electrocautery).
Complications. Patients may experience temporary but severe discomfort in the shoulders after laparoscopy due to residual carbon dioxide gas that puts pressure on the diaphragm. The incisions, even with laparoscopy, may cause pain afterward, which can usually be treated effectively with mild pain relievers. There are small risks for bleeding, infection, and reaction to anesthesia.
Recurrence. Even with very successful surgery, endometriosis may recur within several months to several years.
Hysterectomy
Hysterectomy is the surgical removal of the uterus. Endometriosis accounts for a significant percentage of these procedures. Hysterectomy does not, however, necessarily cure endometriosis.
A woman cannot become pregnant after having a hysterectomy. Women should realize that hysterectomy causes immediate menopause if the ovaries are removed.
Types of Hysterectomies
Once a decision for a hysterectomy has been made, the patient should discuss with her doctor what will be removed. The common choices are:
- Total Hysterectomy (Removal of uterus and cervix). Removing only the uterus with hysterectomy has the same risk for recurrence as conservative surgery. Subtotal hysterectomy involves removing the uterus but keeping the cervix intact.
- Bilateral Oophorectomy (Removal of both ovaries) or Bilateral Salpingo-Oophorectomy (Removal of the fallopian tubes and ovaries). For endometriosis treatment, removal of the ovaries is often performed in combination with hysterectomy. This is the only potential cure for endometriosis. If endometriosis has developed outside the uterus then even ovary removal procedures are not curative.
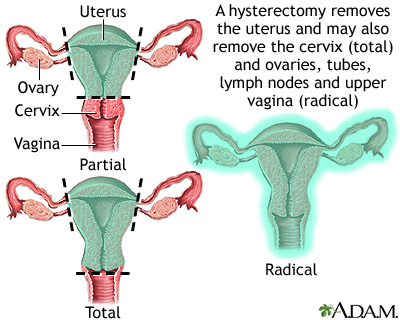
Removal of the ovaries (oophorectomy) along with hysterectomy significantly reduces the likelihood that endometriosis will recur. However, there is still a small chance that recurrence can happen.
Types of Hysterectomy Procedures
Hysterectomies may be performed abdominally (through an incision in the abdomen) or vaginally (through a vaginal incision). A variation of the vaginal approach is called laparoscopic-assisted vaginal hysterectomy (LAVH). There are other laparoscopic approaches as well.
Recovery times for vaginal hysterectomy and LAVH are shorter than those for abdominal hysterectomy. However, hospital stays may be longer with LAVH than standard vaginal hysterectomy. It is not clear whether LAVH adds any significant benefits compared to the standard vaginal procedure. Abdominal hysterectomy is still the most commonly performed procedure.
After Hysterectomy
The ovaries are the main source of production of estrogen. In premenopausal woman, the removal of ovaries causes premature menopause. After hysterectomy with bilateral oophorectomy, women may have hot flashes and other symptoms of menopause, including vaginal dryness, insomnia, and weight gain. Women who have surgical removal of both ovaries, and who do not receive hormone replacement therapy, tend to have more severe hot flashes than women who enter menopause naturally..
If hormone replacement therapy (HRT) is recommended after hysterectomy and ovary removal, it is given as estrogen-only replacement therapy (ERT). (Women without ovaries do not need to take combination estrogen-progesterone HRT.)
After a total hysterectomy, in which the cervix has been removed, a woman does not need annual Pap smears of the cervix. However, she still should get regular pelvic and breast exams.
Resources
- www.asrm.com -- American Society for Reproductive Medicine
- www.acog.org -- American College of Obstetricians and Gynecologists
- www.womenshealth.gov -- National Women's Health Information Center
- www.endometriosis.org -- Endometriosis.org
- www.resolve.org -- National Infertility Association
References
Brown J, Pan A, Hart RJ. Gonadotrophin-releasing hormone analogues for pain associated with endometriosis. Cochrane Database Syst Rev. 2010 Dec 8;(12):CD008475.
Bulun SE. Endometriosis. N Engl J Med. 2009 Jan 15;360(3):268-79.
Daniels J, Gray R, Hills RK, Latthe P, Buckley L, Gupta J, et al. Laparoscopic uterosacral nerve ablation for alleviating chronic pelvic pain: a randomized controlled trial. JAMA. 2009 Sep 2;302(9):955-61.
Davis L, Kennedy SS, Moore J, Prentice A. Modern combined oral contraceptives for pain associated with endometriosis. Cochrane Database Syst Rev. 2007 Jul 18;(3):CD001019.
de Ziegler D, Borghese B, Chapron C. Endometriosis and infertility: pathophysiology and management. Lancet. 2010 Aug 28;376(9742):730-8.
Division of Reproductive Health, National Center for Chronic Disease Prevention and Health Promotion; Centers for Disease Control and Prevention (CDC), Farr S, Folger SG, Paulen M, et al. U S. Medical Eligibility Criteria for Contraceptive Use, 2010: adapted from the World Health Organization Medical Eligibility Criteria for Contraceptive Use, 4th edition. MMWR Recomm Rep. 2010 Jun 18;59(RR-4):1-86.
Falcone T, Lebovic DI. Clinical management of endometriosis. Obstet Gynecol. 2011 Sep;118(3):691-705.
Flower A, Liu JP, Chen S, Lewith G, Little P. Chinese herbal medicine for endometriosis. Cochrane Database Syst Rev. 2009 Jul 8;(3):CD006568.
Giudice LC. Clinical practice. Endometriosis. N Engl J Med. 2010 Jun 24;362(25):2389-98.
Jacobson TZ, Duffy JM, Barlow D, Farquhar C, Koninckx PR, Olive D. Laparoscopic surgery for subfertility associated with endometriosis. Cochrane Database Syst Rev. 2010 Jan 20;(1):CD001398.
Jacobson TZ, Duffy JM, Barlow D, Farquhar C, Koninckx PR, Olive D. Laparoscopic surgery for subfertility associated with endometriosis. Cochrane Database Syst Rev. 2010 Jan 20;(1):CD001398.
Lobo RA. Endometriosis. Etiology, pathology, diagnosis, management. Katz VL, Lobo RA, Lentz G, Gershenson D, eds. Comprehensive Gynecology. 5th ed. St. Louis, MO: Mosby; 2007: chap 19.
[No authors listed] ACOG Practice Bulletin No. 110: noncontraceptive uses of hormonal contraceptives. Obstet Gynecol. 2010 Jan;115(1):206-18.
Ortiz DD. Chronic pelvic pain in women. Am Fam Physician. 2008 Jun 1;77(11):1535-42.
Parker WH, Broder MS, Chang E, Feskanich D, Farquhar C, Liu Z, et al. Ovarian conservation at the time of hysterectomy and long-term health outcomes in the nurses' health study. Obstet Gynecol. 2009 May;113(5):1027-37.
Shakiba K, Bena JF, McGill KM, Minger J, Falcone T. Surgical treatment of endometriosis: a 7-year follow-up on the requirement for further surgery. Obstet Gynecol. 2008 Jun;111(6):1285-92.
|
Review Date:
9/10/2012 Reviewed By: Harvey Simon, MD, Editor-in-Chief, Associate Professor of Medicine, Harvard Medical School; Physician, Massachusetts General Hospital. Also reviewed by David Zieve, MD, MHA, Medical Director, A.D.A.M., Inc. |







